Cardiovascular diseases remain a leading cause of mortality globally.
When patients experience chest discomfort or palpitations, the first diagnostic tool a doctor reaches for is the Electrocardiogram (ECG).
Many patients undergo this test, assuming it will provide a definitive answer about the state of their arteries.
A common question we encounter at our Health screening centre in Bangalore is whether a simple ECG can confirm a blockage in the heart.
The answer is nuanced.
While an ECG is an invaluable tool for monitoring heart rhythm and electrical activity, it has specific limitations when it comes to detecting physical obstructions in the coronary arteries.
It is possible to have a normal resting ECG even with significant arterial blockage.
Understanding the capabilities and limitations of this test is crucial for anyone concerned about their heart health.
This guide explores how an ECG for heart blockage works, what the electrocardiogram test results actually show, and why it is often just the first step in a comprehensive cardiac evaluation.
Medical Disclaimer
The information provided in this blog regarding ecg for heart blockage and cardiac health is for general educational purposes only. It does not constitute professional medical advice, diagnosis, or treatment.
Heart conditions can present with vague or silent symptoms. Do not use this article to self-diagnose.
Always consult a qualified cardiologist or visit a certified Health screening centre in Bangalore for an accurate diagnosis.
If you experience chest pain, shortness of breath, or severe discomfort, seek emergency medical attention immediately.
Understanding the Mechanism: How an ECG Works
To understand why an ECG might miss a blockage, one must first understand what the test actually measures.
The human heart operates on an internal electrical system.
Each heartbeat begins with an electrical impulse generated by the Sinoatrial (SA) node.
This impulse travels through the heart muscle, causing it to contract and pump blood to the rest of the body.
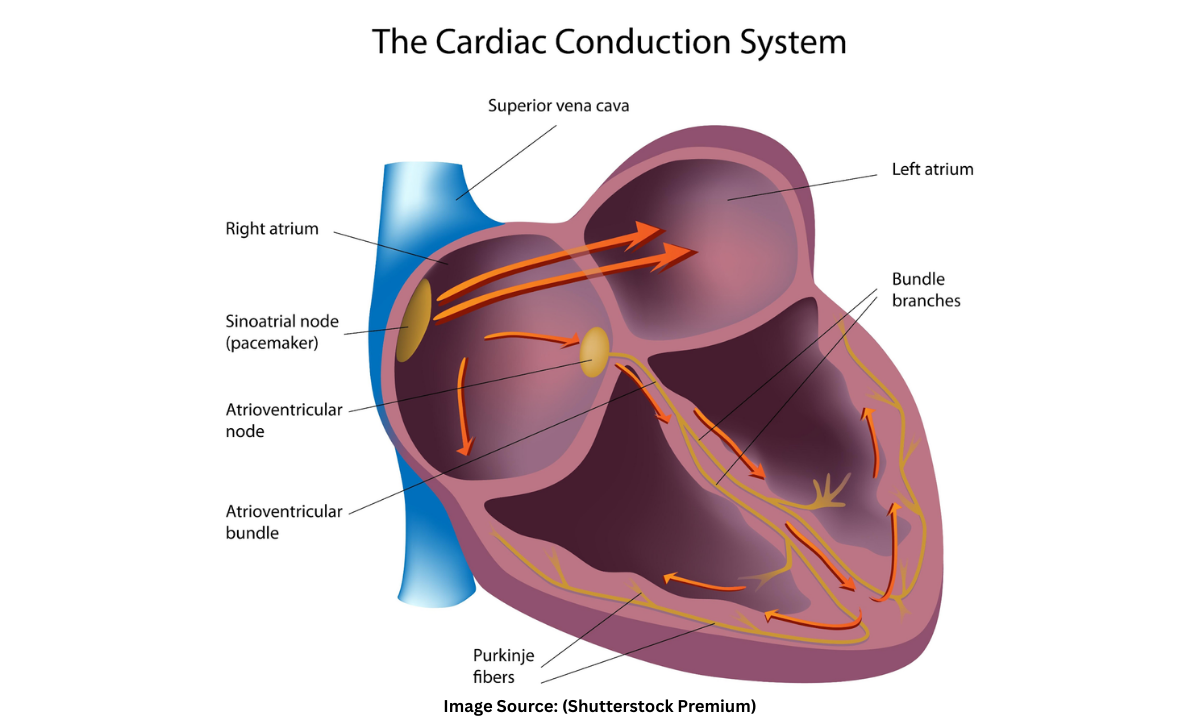
An electrocardiogram (ECG) records this electrical activity. During the test, electrodes are placed on the skin of the chest, arms, and legs.
These sensors detect the tiny electrical changes on the skin that arise from the heart muscle’s electrophysiologic pattern of depolarizing and repolarizing during each heartbeat.
The machine translates these signals into a graph of waves.
- P wave: Represents atrial depolarization (upper chambers contracting).
- QRS complex: Represents ventricular depolarization (lower chambers contracting).
- T wave: Represents ventricular repolarization (heart relaxing).
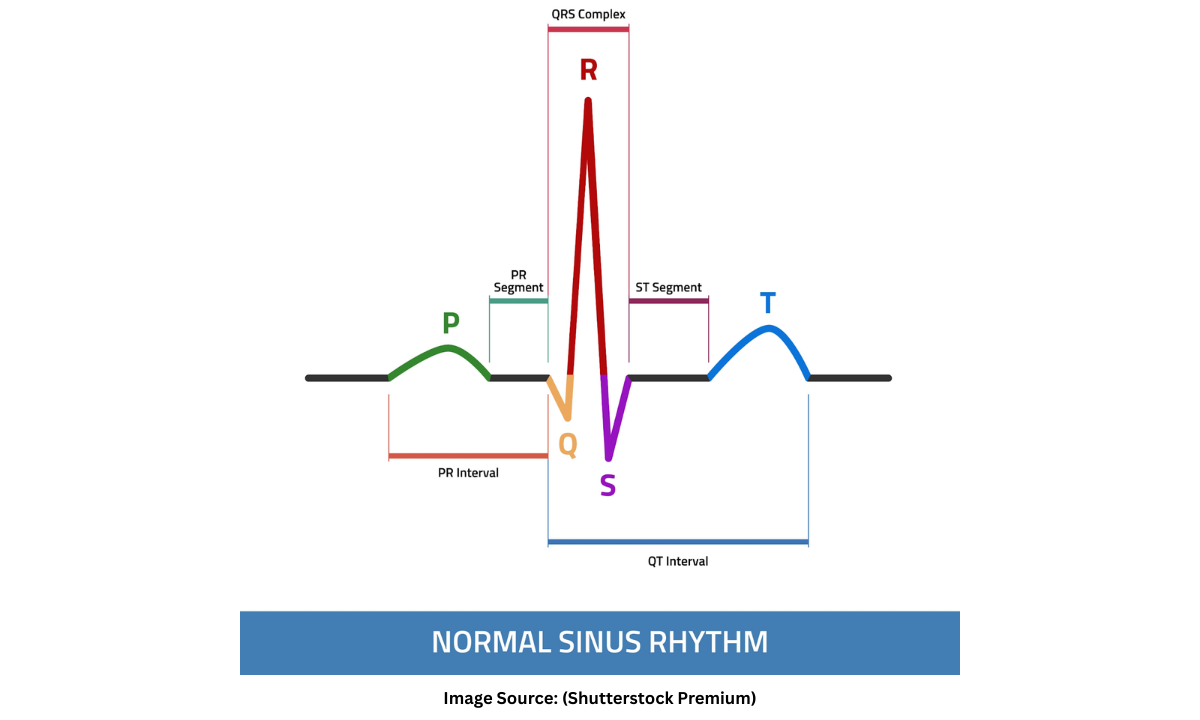
Doctors analyze the shape, timing, and duration of these waves.
Any deviation from the standard pattern indicates a disruption in the heart’s electrical conduction or physical structure.
For more information, read our blog:
What Is An Electrocardiogram Test And How Does It Work?
Can an ECG Detect Heart Blockage?
The term heart blockage is often used interchangeably by patients to describe two completely different medical conditions.
- Electrical Heart Block: A delay or interruption in the electrical signal traveling through the heart.
- Coronary Artery Disease (CAD): A physical buildup of plaque (atherosclerosis) inside the arteries that supply blood to the heart.
Detecting Electrical Heart Block
Yes. An ecg for heart blockage is the gold standard for diagnosing electrical blocks.
If the electrical signal is delayed at the AV node or fails to reach the ventricles, the ECG strip will show a prolonged gap between the P wave and the QRS complex.
This allows doctors to diagnose conditions like First-Degree, Second-Degree, or Third-Degree Heart Block immediately.
Detecting Coronary Artery Blockage (Physical Block)
Not always.
This is where the limitation lies. A resting ECG only records the heart’s electrical activity at that specific moment.
If a patient has a 70% physical blockage in a coronary artery but is resting comfortably, the blood flow might still be sufficient to keep the heart muscle alive and functioning.
In this state, the electrical patterns may appear completely normal.
The ECG typically detects a physical blockage only under two conditions:
- Active Ischemia: The heart muscle is currently starved of oxygen, causing ST-segment depression on the graph.
- Previous Myocardial Infarction: The patient has had a heart attack in the past, leaving scar tissue that does not conduct electricity, causing pathological Q waves.
Therefore, a Normal ECG does not guarantee that the arteries are free of cholesterol plaque. It simply means the heart is not currently suffering from acute electrical distress.
Interpreting Electrocardiogram Test Results
Patients often receive their ECG report and attempt to decipher the complex grid of lines before consulting a doctor.
While a definitive interpretation requires the expertise of a cardiologist, understanding the fundamental components of electrocardiogram test results provides valuable insight into cardiac health.
A standard 12-lead ECG provides twelve distinct electrical views of the heart.
The results generally fall into three primary categories based on the shape and timing of the waves.
A. Normal Sinus Rhythm
This is the medical term for a healthy, functioning heartbeat.
A normal report typically displays the following characteristics:
- Rate: The heart beats at a steady pace between 60 and 100 beats per minute.
- Rhythm: The distance between consecutive heartbeats (R-R interval) is constant and regular.
- Conduction: The electrical impulse travels smoothly from the upper chambers (atria) to the lower chambers (ventricles) without any delay or block.
A finding of “Normal Sinus Rhythm” confirms that the heart’s electrical system is currently operating within standard parameters.
However, it is important to note that a normal resting result does not guarantee the absence of physical blockages, as the heart may not be under stress during the test.
B. Signs of Ischemia (Reduced Blood Flow)
If a coronary artery is partially blocked by plaque, the heart muscle may struggle to receive adequate oxygen.
This condition is known as ischemia and often appears on the graph as specific deviations.
- ST-Segment Depression: The line connecting the QRS complex and the T wave dips below the baseline.
- T-Wave Inversion: The T wave, which is normally upright, flips upside down.
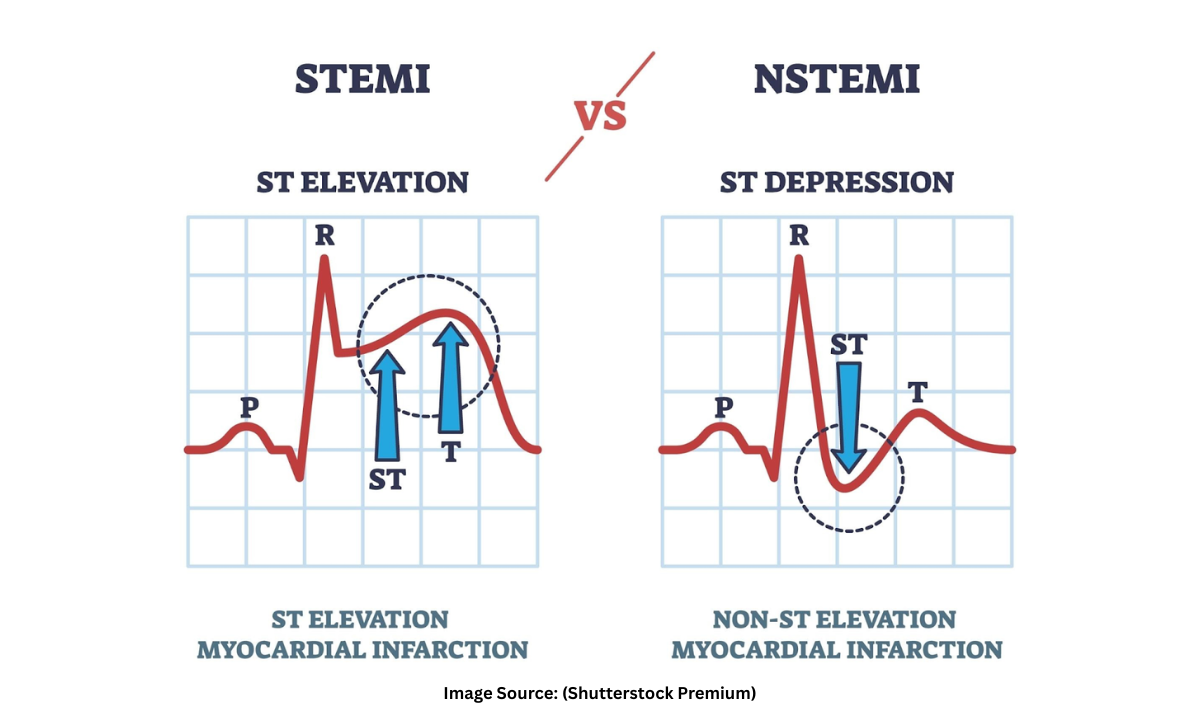
These abnormalities indicate that the heart muscle is starving for oxygen.
The presence of these signs usually prompts further investigation, such as an angiogram, to determine the exact location and severity of the restricted blood flow.
C. Signs of Infarction
If a blockage completely obstructs blood flow, the heart muscle begins to die.
This is clinically termed a myocardial infarction or heart attack.
The ECG captures specific markers of this damage.
- ST-Elevation: A distinct rise in the ST segment above the baseline indicates an acute, ongoing heart attack.
- Pathological Q Waves: Deep and wide Q waves suggest that a heart attack occurred in the past and has left permanent scar tissue on the heart wall.
The detection of ST-elevation is a critical medical emergency.
It signifies that a major artery is 100% blocked, requiring immediate intervention to restore blood flow and save the heart muscle from irreversible necrosis.
When Should You Get an ECG?
As an ECG is non-invasive and painless, it is the primary screening tool for anyone presenting with potential cardiac issues.
Doctors recommend an ECG test in Bangalore immediately if you experience specific heart blockage symptoms.
Primary Symptoms
The body often provides clear signals when the heart is in distress.
- Angina (Chest Pain): A squeezing, pressure-like sensation in the centre of the chest. This pain often radiates to the left arm, jaw, neck, or back.
- Dyspnea (Shortness of Breath): Difficulty breathing, especially during physical exertion or when lying flat.
- Palpitations: A rapid, fluttering, or pounding heartbeat that occurs without exercise.
- Syncope (Fainting): Sudden loss of consciousness or severe dizziness, which may indicate a dangerous drop in heart rate or a blockage.
These symptoms serve as critical warning signs that the heart muscle is under stress.
If you experience any of these indicators, seeking immediate medical attention is vital to prevent permanent damage or a cardiac event.
Silent Ischemia Risk Factors
Some patients, particularly diabetics, may have severe heart blockages without feeling any chest pain.
This condition is known as Silent Ischemia.
For these high-risk individuals, regular screening is essential even in the absence of obvious symptoms.
- Hypertension: High blood pressure damages arteries over time.
- Diabetes: High blood sugar accelerates plaque buildup.
- High Cholesterol: Excess lipids deposit in the coronary arteries.
- Family History: Genetics play a significant role in susceptibility to heart disease.
Regular ECG screenings for individuals with these risk factors can detect early electrical abnormalities before they manifest as a life-threatening heart attack.
Early detection allows for timely intervention and lifestyle modification.
Beyond the ECG: Next Steps for Diagnosis
If your electrocardiogram test results come back normal but you continue to experience symptoms like chest pain or breathlessness, the diagnostic journey does not end there.
Since a resting ECG often fails to detect blockages that only affect the heart under stress, doctors frequently prescribe advanced tests to unmask the hidden problem.
The following procedures are typically the next logical steps in a cardiac evaluation:
- Treadmill Test (TMT): Also known as a cardiac stress test.
This procedure involves monitoring the heart’s electrical activity while the patient walks on a treadmill.
As physical exertion increases the heart’s demand for oxygen, a blockage that was silent at rest may suddenly appear as an abnormality on the ECG graph.
- Echocardiogram (ECHO): This is an ultrasound of the heart.
It uses sound waves to create a moving image of the heart muscle and valves.
It helps doctors visualize the pumping efficiency (Ejection Fraction) and identify if any part of the heart wall is moving poorly due to a lack of blood flow.
- Coronary Angiogram: This is the gold standard for confirming a blockage.
A contrast dye is injected into the coronary arteries, and X-ray imaging is used to see the exact location and percentage of the obstruction.
It is an invasive procedure but offers the most definitive diagnosis.
These advanced diagnostic tools work in tandem with the initial ECG to provide a complete picture of cardiovascular health.
While the ECG acts as the primary screening filter, tests like the Angiogram provide the detailed roadmap required for treatment planning, whether that involves medication, stenting, or bypass surgery.
Why Choose Koshikaa?
Finding a reliable Health screening centre in Bangalore is the first step toward proactive heart health.
We understand that cardiac issues cannot wait.
Our facility is equipped with state-of-the-art diagnostic technology to ensure that every ECG test in Bangalore is performed with clinical precision.
Why patients trust Koshikaa for their cardiac screening:
- Advanced Technology: We utilize digital 12-lead ECG machines that provide high-resolution data, minimizing artifacts and ensuring accurate wave interpretation.
- Expert Analysis: Every report is generated with precision and reviewed to ensure that even subtle abnormalities in the ST segment or T waves are flagged for medical attention.
- Comprehensive Packages: We believe that an ECG is most effective when paired with other metabolic markers.
Our screening packages often include Lipid Profiles and Fasting Blood Sugar tests to assess the root causes of blockages alongside the electrical activity.
These features ensure that you receive not just a graph, but a complete picture of your heart’s functionality.
By combining ECG services in Bangalore with broader metabolic screening, Koshikaa enables you to detect silent risks like cholesterol spikes or hypertension before they develop into critical heart blockages.
Conclusion
While an Electrocardiogram is an indispensable tool for monitoring heart rhythm and detecting past damage, it is not a standalone detector for all coronary blockages.
A normal ecg for heart blockage in the absence of symptoms is reassuring, but it does not guarantee immunity from coronary artery disease, especially if the blockage is currently stable.
Regular screening at a certified centre such as Koshikaa remains the most effective strategy for early detection.
If you are over the age of 40 or have a family history of cardiac issues, do not wait for symptoms like chest pain to appear.
Schedule a comprehensive heart checkup today to ensure your heart remains as healthy as possible.
Sources:
1 . Fortis Healthcare (Primary Reference): To understand the role of ECG in detecting heart blockages.
https://www.fortishealthcare.com/blogs/understanding-role-ecg-detecting-heart-blockages/
2. American Heart Association (AHA): Electrocardiogram (ECG or EKG) & heart block.
3. Mayo Clinic: Electrocardiogram (ECG) – what it can and cannot find.
https://www.mayoclinic.org/tests-procedures/ekg/about/pac-20384983
4. Cleveland Clinic: Myocardial Ischemia
https://my.clevelandclinic.org/health/diagnostics/16953-electrocardiogram-ekg
5. Koshikaa: Client profiling.