Heart attacks rarely happen overnight.
They are usually a slow, silent process that takes years. Imagine your arteries are the “Water Pipes” of your house.
Over time, grease and rust can build up inside them. At first, the water still flowed fine. But as the layer gets thicker, the pipe narrows, and eventually, it clogs completely.
In your body, that “Grease” is Cholesterol.
Conditions like atherosclerosis—where plaque builds up inside the arteries—can restrict blood flow without showing early symptoms.
The Lipid Profile Test is the only way to look inside your pipes. It measures the amount of fat (lipids) in your blood to tell you if your system is flowing freely or slowly clogging up.
According to medical standards this is a comprehensive panel of blood tests used to find abnormalities in lipids (cholesterol and triglycerides).
It is the primary diagnostic tool used to assess an individual’s risk of developing coronary artery disease, heart attack, or stroke.
In this guide, we will decode the lipid profile report, explain the good vs. the bad cholesterol, and show you the real lipid profile test price in Bangalore so you can protect your heart without overpaying.
What is the Lipid Profile Test?

Understanding the medical definition and biological function.
To interpret the results correctly, it is essential to understand what is being measured in the blood.
A Lipid Profile (also known as a Lipid Panel) measures the concentration of specific fat molecules called lipoproteins in the blood.
- Lipids are fatty, wax-like substances found in the body. While the body needs lipids for cell growth and energy, excess levels can be harmful.
- Because lipids are insoluble in water (and blood), they must be transported by protein carriers. These combinations of fat and protein are called Lipoproteins.
The test does not just measure “fat”; it quantifies the different types of lipoproteins based on their density and function.
- Low-Density Lipoprotein (LDL): Often referred to clinically as “bad cholesterol,” this lipoprotein deposits cholesterol into the arterial walls, leading to plaque formation.
- High-Density Lipoprotein (HDL): Known as “good cholesterol,” this lipoprotein absorbs excess cholesterol and carries it back to the liver for removal.
- Triglycerides: A type of fat (lipid) found in the blood. The body converts excess calories from food into triglycerides, which are stored in fat cells for energy.
The primary lipid profile means of assessment is to detect Dyslipidemia—an abnormal amount of lipids in the blood.
This condition is a major risk factor for cardiovascular disease (CVD) and pancreatitis.
The 4 Key Parameters
What exactly are we measuring in your blood?
A standard Lipid Profile does not just measure “Fat.” It breaks down the total lipid concentration into four distinct components. Each plays a specific physiological role in your metabolism.
1. Low-Density Lipoprotein (LDL)
- The Clinical Name: Often termed “Bad Cholesterol,” but scientifically, it is the primary transporter of cholesterol to peripheral tissues.
- The Mechanism: LDL particles carry cholesterol from the liver to the cells that need it for membrane repair.
- The Risk: If LDL levels are excessive, the cells stop accepting it. The excess LDL then infiltrates the inner walls of the arteries (endothelium). There, it oxidizes and triggers an inflammatory response, forming a hard deposit called Plaque. This process is known as Atherosclerosis.
- Key Metric: This is the most critical parameter for assessing heart attack risk.
2. High-Density Lipoprotein (HDL)
- The Clinical Name: “Good Cholesterol.”
- The Mechanism: HDL acts as a scavenger. It performs a process called Reverse Cholesterol Transport. It travels through the bloodstream, picks up excess cholesterol from the arterial walls, and transports it back to the liver to be broken down and excreted.
- The Benefit: High levels of HDL are cardioprotective. They actively reduce the risk of plaque formation.
3. Triglycerides (TG)
- The Definition: Triglycerides are the most common type of fat in the body. They are energy storage units.
- The Source: When you eat more calories than you burn (especially from sugar, alcohol, or refined carbs), the liver converts the excess energy into triglycerides and stores them in adipose tissue (fat cells).
- The Risk: Unlike cholesterol (which builds cells), high triglycerides thicken the blood and, in extreme cases, can cause Pancreatitis (inflammation of the pancreas).
4. Total Cholesterol
The Formula: It is not a separate molecule but a calculated sum:
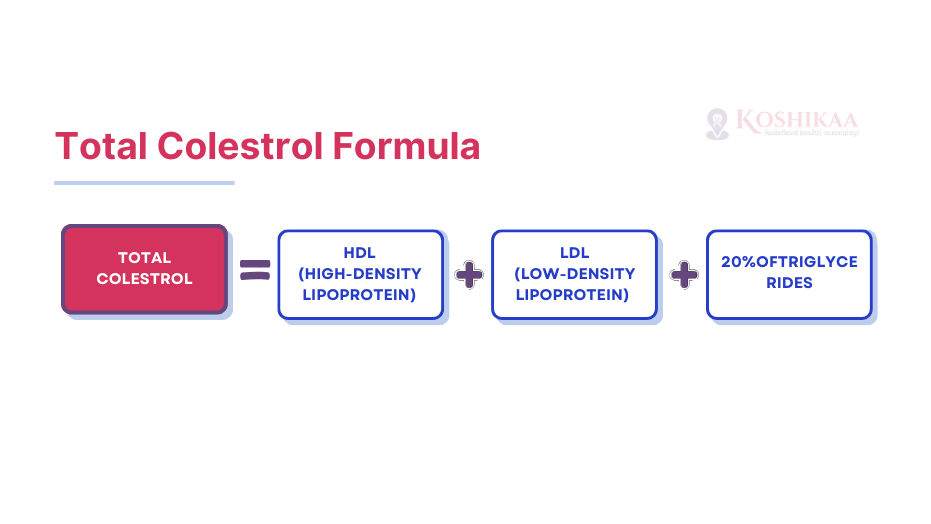
- The Purpose: It provides a “Gross Estimate” of lipid health, but it is less precise than looking at the LDL/HDL ratio specifically.
Note on VLDL: Your report might also mention VLDL (Very Low-Density Lipoprotein). This is a precursor to LDL and primarily carries triglycerides. It is usually calculated mathematically rather than measured directly.
Why is the Test Used?

Is this test for everyone, or just for heart patients?
Doctors use the Lipid Profile Test for three primary medical reasons. It is not just about finding “bad news”; it is about prevention.
A. The Early Warning System
- Goal: To detect risks before symptoms appear.
- Guideline: According to the National Heart, Lung, and Blood Institute, healthy adults aged 20 and older should get a lipid profile every 4 to 6 years.
- High Risk: If you have diabetes, hypertension, or a family history of heart disease, you may need it yearly.
B. Monitoring: The Progress Report
- Goal: To check if your medication or diet is working.
- Scenario: If you are taking Statins (cholesterol-lowering drugs), this test tells the doctor if the dosage needs adjustment.
C. Diagnosis Finding the Root Cause
- Goal: To diagnose specific conditions unrelated to the heart.
- Example: Extremely high triglycerides can be a sign of Pancreatitis (inflammation of the pancreas) or Hypothyroidism.
Who Should Get Tested?
If you tick more than one box below, you should book a lipid profile check immediately.
- Smoker: Chemicals in smoke lower your “Good” HDL.
- Diabetic/Pre-diabetic: High blood sugar damages artery walls, making it easier for LDL to stick.
- Overweight: BMI > 25 (or waistline > 35 inches for women, > 40 for men).
- Family History: A parent or sibling had a heart attack before age 55.
- Sedentary Lifestyle: You sit for more than 8 hours a day.
Preparation: The Strict Fasting Rule
Why does the lab insist on you starving?
The Lipid Profile Test is highly sensitive to food. When you eat, your liver produces Chylomicrons (microscopic fat particles) to transport energy from food.
These particles stay in your blood for hours, artificially spiking your Triglyceride count.
To get an accurate “baseline,” we need these particles to clear out.
The Protocol: 9 to 12 Hours Fasting
| Category | The Rule | The Reason |
|---|---|---|
| Food | STRICTLY NO. Not even a biscuit or a mint. | Even small sugars trigger insulin and lipid release. |
| Water | YES. Drink plenty of plain water. | Hydration helps the phlebotomist find your vein easily. |
| Coffee/Tea | NO. (Even black coffee). | Caffeine can slightly alter metabolic rates. |
| Alcohol | NO (for 24 hours). | Alcohol is metabolized directly into Triglycerides. A drink last night = High result today. |
| Medication | YES. (Unless the doctor says otherwise). | Do not skip your BP or Diabetes medicines. |
Smart Tip: Since you need to fast for ~10 hours, the best time to book your Blood test in Bengaluru is early morning (e.g., 7:00 AM or 8:00 AM). This way, you sleep through most of the fasting period!
Decoding Your Report
Your report will be full of numbers. Here is how to read them.
A lipid profile report typically measures values in mg/dL (milligrams per deciliter).
Instead of panicking over every digit, use this “Traffic Light” system to understand where you stand.
Table: Standard Lipid Profile Reference Ranges (Adults)
| Parameter | Normal (Safe) | High Risk (Danger) | |
|---|---|---|---|
| Total Cholesterol | Less than 200 mg/dL | 200 – 239 mg/dL | 240 mg/dL and above |
| LDL (Bad) | Less than 100 mg/dL | 130 – 159 mg/dL | 160 mg/dL and above |
| HDL (Good) | 60 mg/dL or higher | 40 – 59 mg/dL | Less than 40 mg/dL (Too Low) |
| Triglycerides | Less than 150 mg/dL | 150 – 199 mg/dL | 200 mg/dL and above |
Key Takeaways from the Numbers:
- HDL is Opposite: For HDL, Higher is Better.
- If your HDL is < 40, it is considered a major risk factor for heart disease, even if your total cholesterol is normal.
- If your HDL is > 60, it acts as a “Negative Risk Factor,” effectively cancelling out one bad risk factor!
- The LDL Target: If you already have diabetes or a history of heart issues, your doctor might want your LDL strictly below 70 mg/dL, not just 100.
- The “Hidden” Ratio:
- Look at the ratio of Total Cholesterol ÷ HDL.
- Ideally, this number should be below 5. If it is above 5, your risk of a blockage is significantly higher.
Important: Different labs use different machines. Always refer to the specific “Reference Range” printed on the right side of your lipid profile report from Koshikaa or any other lab.
Lipid Profile Test Price in Bangalore
The cost of healthcare often includes more than just the bill—it includes traffic, waiting time, and fuel.
When looking for a lipid profile test price, you will find a wide range.
Some hospitals charge premium rates for the “Brand,” while local centers might lack NABL accreditation.
Here is the 2026 market estimate for lipid profile test price in Bangalore:
The Price Watch Table
| Provider Type | Estimated Cost | Hidden Costs | |
|---|---|---|---|
| Big Hospital Labs | ₹700 – ₹1,200 | Parking fees + Registration waits | 12 – 24 Hours |
| Local Diagnostic Centers | ₹400 – ₹600 | Travel stress (Traffic) | Varies |
| Koshikaa (Home & Lab Collection) | ₹399 – ₹349 | None | 6 – 8 Hours |
Most people don’t just book a Lipid Profile alone. Check Koshikaa’s Heart Health Package or Full Body Checkup. For just a slightly higher price (e.g., ₹899–₹1299), you often get the Lipid Profile PLUS HbA1c, Thyroid, and Kidney tests. It offers 3x the value.
Why Book a “Blood Test in Bengaluru” at Home?
The “Fasting” factor makes home collection the winner.
Remember, you need to be fasting for 10–12 hours.
- Option A (Lab Visit): You wake up hungry, drive through Bangalore traffic (adding stress), find parking, and wait in a queue while starving.
- Option B (Koshikaa Home Visit): You wake up, relax in your armchair, and our phlebotomist arrives at 7:00 AM. Sample taken in 5 minutes. You can eat breakfast immediately.
How to Book in 3 Steps:
- Search: Look for “Lipid Profile” or “Heart Checkup” on the Koshikaa Website.
- Schedule: Choose a morning slot (6:30 AM – 9:00 AM) that suits your fasting schedule.
- Relax: Our vaccinated, NABL-trained professional arrives at your doorstep.
Conclusion
Your body is a complex engine, and your blood is the fuel line. You wouldn’t drive your car for years without checking the oil, yet many of us ignore our lipid profile test until a doctor forces us to take it.
Here is the truth: High cholesterol has zero symptoms. You won’t feel pain, you won’t feel dizzy, and you won’t feel “clogged” until it is often too late. The only way to know the truth is to look at the numbers.
Whether your lipid profile report shows a need for a lifestyle U-turn or gives you a green signal, knowing where you stand is the most powerful thing you can do for your heart. At Koshikaa, we make that first step effortless. With our Blood test in Bengaluru home collection service, you can protect your heart without leaving your home.
Don’t wait for a warning sign. Book your checkup today, because the best time to fix a roof is when the sun is shining.
Frequently Asked Questions (FAQs)
Q1: Can thin people have high cholesterol?
YES. This is the biggest myth about heart health. Cholesterol isn’t just about how much fat you eat; it’s about how your liver processes it. Even if you are skinny, genetic conditions (like Familial Hypercholesterolemia) can cause your liver to overproduce bad cholesterol. You can be thin on the outside but “fat on the inside.”
Q2: Does stress affect my lipid profile results?
Indirectly, Yes. Chronic stress releases a hormone called Cortisol. High cortisol levels can trigger your liver to produce more “bad” cholesterol (LDL) and lower your “good” cholesterol (HDL). If you have been under severe stress for months, your numbers might be slightly elevated.
Q3: What is the difference between VLDL and LDL?
Think of them as two different types of “Delivery Trucks.”
- VLDL (Very Low-Density Lipoprotein): Mainly carries Triglycerides (fat for energy) to your tissues.
- LDL (Low-Density Lipoprotein): Mainly carries Cholesterol (for cell repair).
- Both are considered “bad” because, in high amounts, they both contribute to plaque buildup in arteries.
Q4: How can I naturally improve my Lipid Profile?
Before starting medication, doctors often suggest the “3-Month Rule” for borderline cases:
- Eat Soluble Fiber: Oats, beans, and apples act like a sponge that soaks up cholesterol in your gut.
- Move More: 30 minutes of brisk walking daily is the only natural way to significantly raise your “Good” HDL.
- Cut Trans Fats: Avoid bakery items (puffs, biscuits) and fried foods entirely.
Q5: How often should I get a Lipid Profile test?
- Healthy Adults (20+): Once every 4–5 years.
- High Risk (Diabetic, Smoker, Family History): Once every year.
- On Medication: Every 3–6 months to check if the dosage is working.
Sources:
- Primary Data: Medical & Scientific Authorities.
- MedlinePlus – Lipid Panel
- National Heart, Lung, and Blood Institute (NHLBI): NHLBI – Blood Cholesterol
- Cleveland Clinic: Cleveland Clinic – Lipid Panel
- Clinical Guidelines & Ranges: NCEP ATP III guidelines from National Cholesterol Education Program (NCEP)
- Regional & Market Data: Apollo Hospitals – Lipid Profile Test